What Is Physician Burnout Reduction?
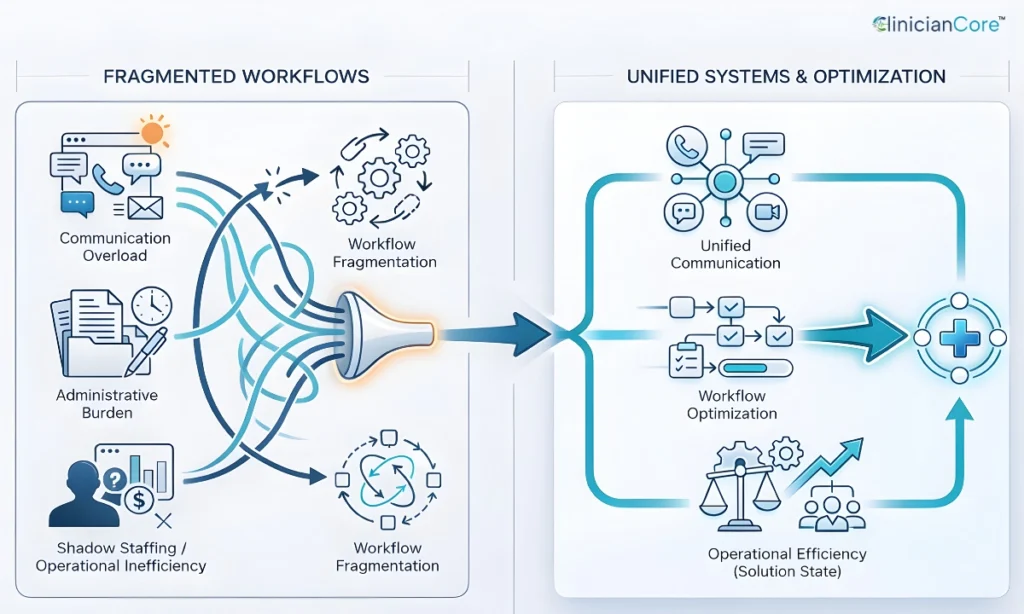
Physician Burnout Reduction is the operational strategy of systematically removing administrative friction and cognitive load at scale for healthcare organizations. Unlike wellness initiatives which focus on individual resilience, reduction strategies target root causes: inefficient technology, fragmented communication, and excessive documentation.
For Executives: The Financial Reality
This is not an HR issue; it is a P&L issue. Burnout is the leading indicator of “Shadow Staffing” costs and revenue leakage. To understand the full financial urgency, quantify your specific exposure with our Physician Retention & Turnover Cost Calculator.
The State of Healthcare Provider Burnout in 2026
As we move through 2026, the data confirms that burnout is not distributed equally. It is concentrated in high-friction environments where communication is constant.
Burnout Rates by Specialty (Data Snapshot)
High-communication specialties—those requiring constant coordination—continue to report the highest levels of exhaustion.
| Specialty | Burnout Rate (2024 Est.) | Primary Stressor |
| Emergency Medicine | 63% | High-acuity communication loops |
| Ob/Gyn | 53% | After-hours patient messaging |
| Oncology | 53% | Emotional fatigue & care coordination |
| Family Medicine | 51% | Administrative/EHR documentation |
source: AMA
Communication Fatigue as a Systemic Risk
The common thread among the highest-stress specialties is “Communication Fatigue”—the mental drain caused by managing disjointed information across multiple platforms. This fragmentation prevents Communication efficiency and directly correlates with higher error rates.
Causes of Physician Burnout Are Systemic, Not Personal
To solve the crisis, healthcare leadership must recognize that the primary causes of physician burnout are found in the environment, not the individual.
Administrative Burden and EHR Click Fatigue
“Click fatigue” has become a clinical diagnosis in all but name. Physicians today spend a disproportionate amount of their shifts navigating EHR inefficiencies. When technology adds steps to a doctor’s day rather than subtracting them, it degrades the overall Healthcare operations strategy.
Communication Overload in Clinical Teams
Fragmented paging systems, unsecured SMS, and constant “notification pings” fracture a clinician’s attention. This cognitive switching—moving from patient care to a legacy pager and back—is a leading driver of mental exhaustion.
Organizational Physician Burnout Symptoms (Beyond Individual Exhaustion)
While individual physician burnout symptoms include exhaustion and cynicism, an organization displays different red flags that impact viability.
Financial Indicators
Burnout is expensive. The cost of replacing a single physician is often hidden in recruitment and ramp-up time.
| Metric | Estimated Cost Impact |
| Cost of Physician Turnover | $500,000 – $1,000,000 per physician (Recruitment + Lost Revenue) |
Clinical Risk Indicators
Fatigued providers are prone to slip-ups in documentation and prescription. We see a direct correlation between high burnout scores and increased medical errors, which raises liability premiums.
Workforce Stability Indicators
- Rising Turnover: A revolving door of clinicians destabilizes care teams.
- “Shadow Staffing”: The need to hire excess temporary staff to cover the productivity gaps of burnt-out permanent physicians.
Strategic Pillars for Physician Burnout Reduction
Operational Efficiency and Workflow Optimization
The most direct “Side Door” to reducing burnout is through unified communication. By implementing platforms that consolidate messaging, paging, and patient data into a single interface, organizations can return minutes—and mental clarity—to their doctors.
True physician burnout reduction requires fixing the systems clinicians work within. Explore proven organizational solutions for physician burnout that eliminate administrative friction and communication overload at scale.
Leadership and Cultural Accountability
Strategic reduction requires a shift from “wellness apps” to “workflow audits.” Leadership must champion the removal of low-value tasks and empower physicians to influence the technology they use daily.
Next Steps for Executives: Quantify Your Opportunity
You cannot yoga your way out of a broken workflow. Sustainable reduction requires a commitment to better systems—and the financial data to back it up.
Stop guessing the cost of inefficiency. Use our Annual Saving Cost Calculator to input your organization’s data and see exactly how much revenue you can reclaim by eliminating administrative friction today.
Key Takeaways
- Physician Burnout Reduction is an operational strategy not a wellness initiative, focused on removing systemic friction, administrative redundancy, and cognitive load at scale.
- Specialty-Specific Risk: Healthcare provider burnout is not distributed equally; it is highest in communication-intensive fields like Emergency Medicine (63%) and Ob/Gyn (53%), where coordination loops are constant.
- Systemic Root Causes: The primary causes of physician burnout are environmental: “click fatigue” from inefficient EHRs, “communication fatigue” from fragmented paging, and excessive administrative documentation.
- Organizational Symptoms: Beyond individual exhaustion, physician burnout symptoms manifest organizationally as “shadow staffing” costs, rising turnover, and increased clinical error rates that raise liability premiums.
- The Solution Path: Sustainable reduction requires Operational Efficiency and Workflow Optimization. By unifying communication systems and auditing workflows, organizations can reduce cognitive switching and restore clinical focus.
Frequently Asked Questions
What is the most effective way to reduce physician burnout?
The most effective way to reduce physician burnout is through systemic workflow improvements that eliminate administrative burden and communication fragmentation. Rather than focusing on individual resilience, organizations must optimize communication technology and EHR integration.
How does technology impact healthcare provider burnout?
Technology impacts healthcare provider burnout by either increasing cognitive load through poor design or reducing it through automation. Poorly designed EHRs increase “click fatigue,” while unified platforms reduce burnout by streamlining workflows and eliminating redundant manual tasks.
What are the primary drivers of burnout in 2026?
The primary drivers include high administrative volume, “always-on” digital communication expectations, and the lack of interoperability between clinical tools.








