Clinical communication failures occur when critical patient information is delayed, fragmented, misinterpreted, or lost across care teams, directly increasing patient safety risk. According to the National Library of Medicine, patient safety incidents are a global burden: 1 in 10 patients are harmed in healthcare, and the economic cost accounts for 15% of hospital expenditure.
As a Chief Medical Officer and surgeon with 27 years of clinical experience, I’ve witnessed firsthand how these failures compromise patient safety. Clinical communication refers to the exchange of information, ideas, and instructions among healthcare providers, patients, and their families. It encompasses a wide range of interactions, including verbal discussions, written notes, electronic health record (EHR) updates, and telecommunication.
Effective communication is the bedrock of safe, high-quality patient care, ensuring that every member of the care team has a clear, accurate, and up-to-date understanding of a patient’s condition, treatment plan, and progress.
Nearly all clinical communication failures stem from fragmented, non-contextual communication systems. This is why unified clinical communication platforms like ClinicianCore were built specifically to address the root causes of clinical communication failures by enabling secure, context-aware, role-based collaboration across care teams.
The stakes couldn’t be higher. A breakdown in communication can lead to misdiagnoses, delayed treatments, medication errors, and, in severe cases, preventable harm or even death. For healthcare professionals, precision and clarity are paramount in every interaction.
In my 27 years as a surgeon, I have seen firsthand how every detail of communication directly impacts patient outcomes, especially in critical situations like wartime trauma readiness, where clarity can be the difference between life and death.
Examples of Clinical Communication Failures
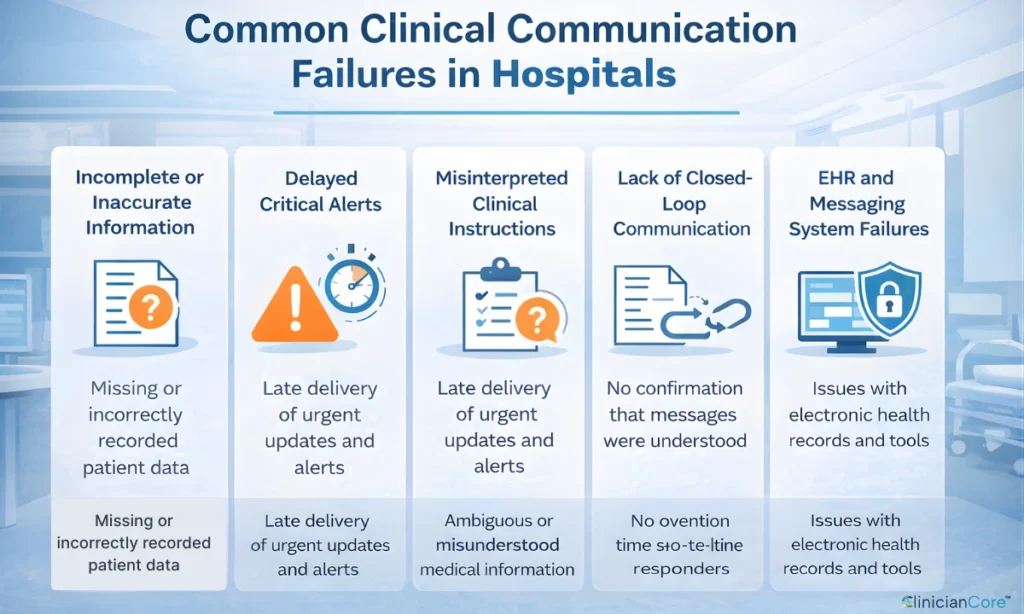
Clinical communication failures can manifest in various forms, each posing distinct risks:
- Incomplete or Inaccurate Information: This occurs when critical patient data, such as allergies, medical history, or current medications, is either missing or incorrectly recorded and transmitted.
- Delayed Communication: Time-sensitive information, like urgent lab results or changes in a patient’s condition, is not relayed promptly, leading to missed opportunities for timely intervention.
- Misinterpretation of Information: Even when information is accurately conveyed, it can be misunderstood by the recipient due to ambiguity, jargon, or a lack of context.
- Lack of Closed-Loop Communication: This failure happens when the sender of information does not confirm that the message has been received and understood by the recipient, leaving room for assumptions and errors.
- Technology-Related Failures: Issues with electronic health records (EHRs), secure clinical communication systems, or other digital tools can hinder effective information exchange.
Verbal handoffs, where information is exchanged face-to-face or over the phone, are particularly susceptible to error due to distractions, incomplete information, or misinterpretation. As a surgeon dedicated to the education and training of residents, I frequently observed the critical challenges inherent in verbal handoffs, where crucial patient details could easily be overlooked amidst the fast-paced demands of clinical practice.
Why Clinical Communication Failures Are Dangerous?
For healthcare leaders, unresolved clinical communication failures quietly erode safety metrics, staff retention, and financial performance, often without triggering immediate alarms. This silent decline impacts hospital boards, risk officers, and CFO-adjacent readers long before a single, catastrophic event makes headlines.
The Devastating Impact of Clinical Communication Failures
Clinical communication failures are one of the leading systemic causes of preventable patient harm, clinician burnout, and operational waste in U.S. hospitals.
- Compromised Patient Safety: Compromised patient safety is arguably the most severe consequence of clinical communication failures. Inaccurate or incomplete information can directly lead to adverse events, delayed diagnoses, and inappropriate treatments.
- Legal and Ethical Ramifications: Communication failures are a leading cause of medical malpractice claims. These failures can lead to significant legal battles, financial penalties, and reputational damage for healthcare providers and institutions. Ethically, a breakdown in communication represents a failure in the duty to provide safe and effective care.
Why Clinical Communication Failures Are Dangerous
- Cause preventable patient harm
- Increase malpractice exposure
- Drive physician burnout
- Create HIPAA compliance risks
What Causes Clinical Communication Failures in Hospitals
- Fragmented tools
- Lack of role-based messaging
- Non-contextual alerts
- Shadow IT and unsecured texting
Financial Implications and Operational Inefficiencies
Beyond patient safety and legal concerns, clinical communication failures impose substantial financial burdens and create operational inefficiencies.
- Increased Operational Costs: Communication failures lead to inefficiencies that drive up healthcare costs. This includes expenses related to redundant tests, extended hospital stays due to preventable errors, and legal costs associated with malpractice suits. These inefficiencies not only impact patient care but also create significant financial strain, prompting clinicians’ efforts to revolutionize healthcare communication for better operational and financial outcomes.
- Wasted Resources: When information is not accurately or timely shared, resources such as staff time, medical supplies, and diagnostic equipment are often misused or duplicated. This not only increases costs but also diverts valuable resources from other critical areas of patient care.
How Clinical Communication Failures Drive Physician Burnout
The constant pressure and frustration stemming from poor communication systems also take a heavy toll on healthcare professionals.
- Physician Burnout: The communication systems are inefficient, and physicians spend valuable time chasing information, making redundant calls, or dealing with avoidable errors. According to the HIPAA Journal, Studies show that 80% of serious medical errors are caused by miscommunication between caregivers. This administrative burden directly contributes to physician burnout, eroding job satisfaction and potentially leading to staff turnover. Having spent 27 years on the front lines of surgery, I understood firsthand how fragmented communication systems contribute to physician frustration and burnout, driving my commitment to developing a unified communication platform to re-engage physicians in their vital work and actively reduce physician burnout.
- Decreased Team Morale: Frequent communication breakdowns can foster an environment of mistrust and frustration among care team members. This can lead to decreased morale, poor teamwork, and a less collaborative work environment.
How Hospitals Can Reduce Clinical Communication Failures
Addressing clinical communication failures requires a multi-faceted approach involving technological solutions, standardized protocols, and ongoing training.
- Implement Secure Unified Clinical Communication Platforms to centralize channels and ensure HIPAA compliance, replacing unsecured personal texting.
- Standardize Communication Protocols, such as SBAR (Situation, Background, Assessment, Recommendation), for consistent handoffs and information exchange.
- Conduct Regular Training and Education for all healthcare professionals on effective communication techniques and the use of communication technologies.
- Promote a Culture of Safety by encouraging an environment where staff feel safe to report communication failures without fear of reprisal.
- Leverage Artificial Intelligence (AI) and Machine Learning (ML) to analyze communication patterns, identify potential gaps, and predict where failures are most likely to occur.
What Healthcare Leaders Should Do Now
Hospital leaders addressing clinical communication failures should:
- Replace fragmented messaging tools with unified platforms
- Eliminate unsecured personal texting
- Enable role-based routing instead of name-based paging
- Integrate secure communication into daily workflows
- Measure communication latency as a patient safety metric
The Path Forward
Clinical communication failures pose a pervasive threat to patient safety, operational efficiency, and the well-being of healthcare professionals. By understanding the various types of failures and their profound impacts, healthcare organizations can implement targeted mitigation strategies.
The integration of advanced communication technologies, coupled with robust training, standardized protocols, and a strong culture of safety, is essential for building a resilient healthcare system. This approach supports greater healthcare interoperability by breaking down communication silos, ensuring that information flows seamlessly between systems and teams. This ultimately leads to better patient outcomes and a more sustainable working environment for all.
As clinical leaders, our responsibility is to move beyond simply documenting care to actively enabling real-time collaboration. The future of medicine hinges on this commitment to unified, reliable clinical communication.
Frequently Asked Questions
Why is clinical communication considered a patient safety issue?
Clinical communication is a patient safety issue because failures in information exchange can lead to delayed treatment, medication errors, missed diagnoses, and preventable adverse events.
How does poor communication contribute to clinician burnout?
Poor communication contributes to clinician burnout because inefficient communication increases cognitive load, alert fatigue, and workflow interruptions, contributing significantly to clinician stress and burnout.
How can hospitals improve clinical communication today?
Hospitals can improve clinical communication by standardizing secure messaging tools, reducing reliance on personal devices, and integrating communication into clinical workflows.
What role does unified communication play in healthcare?
Unified communication platforms centralize secure messaging, alerts, and collaboration tools, reducing fragmentation and improving care coordination.
Why do broken workflows lead to HIPAA violations?
When official tools are too slow or complex, clinicians often resort to unsecure personal devices to send patient data quickly, causing compliance breaches.
Can clinical communication platforms replace the EHR?
No, they are complementary. The EHR is the permanent record of truth, while clinical communication platforms facilitate the real-time collaboration and coordination needed to make decisions that are later documented in the EHR.
What are examples of clinical communication failures in hospitals?
Common examples include incomplete patient handoffs, delayed responses to critical alerts, unsecured personal texting, lack of role-based messaging, and fragmented communication across care teams—each of which increases patient safety ri